75 year old woman with recent right femur neck fracture, intermittent hematuria, right ureteric hydronephrosis and HRCT screening for covid showing fibrotic nodules in right middle lobe
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/ guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
Here is a case I have seen:
A 75 year old woman presented with complaints of Pain in the right thigh
Reduced urine output
Reddish colored urine since 3 days
She stays at home and has 3 children (daughters).
5 years ago, she slipped and fell down the stairs and had a laceration over her forehead for which suturing was done. She even had reduced urine output and hematuria for which she had been evaluated and was diagnosed with Hydroureteronephrosis and UTI for which she was put on medications.
3 years ago, she got diagnosed to be hypertensive and has been on Tab Stamlo 5mg. She is a known case of CKD with anemia. She also started to experience dyspnea on exertion since 3 years on and off, graudal and not progressive, it wasn't associated with cough, PND orthopnea, hemoptysis.3 days ago, she slipped and fell at 4 am and attained right intertrochantric fracture. Since then she has been experiencing reduced urine output and also says she has been having red coloured urine.
General Examination:
The patient is conscious, coherent, and cooperative and oriented to time, place, and person.
Pallor +
When she presented to us she was on foley's inserted by an outside hospital , bright red urine could be seen through her urobag
PR - 90 bpm
Bp - 130/70
RR- 20 cpm
Afebrile
Cvs - S1,S2
Lungs - Inspiratory crackles + in Right IMA , IAA
We've sent routine investigations
We've also taken an orthopedics opinion for her right inter trochanteric fracture
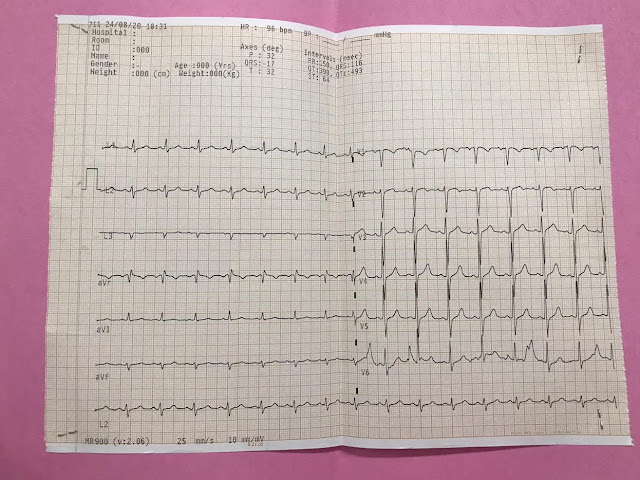
ECG
Problem Assessment :
75 year old woman with
Dyspnea on exertion since 3 years
Right Intertrochanteric fracture since 3 days
Hematuria since 3 days
2Decho was adviced to rule out cardiac cause of Dyspnea
Significant albuminuria - adviced 24 hours urinary protein and creatinine
Usg abdomen showed Right HUN for which urology opinion was taken
For Right ITC fracture for which orthopedics opinion was taken
And also a throat & nasopharyngeal swab was advised keeping the covid pandemic in mind
On Day 2:
Nasopharyngeal swab and throat swab was sent in the morning.
Skin traction to be done as advised by the orthopedics department.
Urology opinion was taken and NCCT KUB was advised
Gynecology opinion was taken to rule out causing cervical and vaginal causes of hematuria. .
On Gynecological evaluation: There is no mass in the abdomen. Since she could not be put in Lithotomy position gynecological examination was not done.
Day 3:
Her swab report came out to be negative
Her sputum sample was sent for cultures and for AFB
Her long standing dyspnea on exertion was because of LAD territory ischaemia
She has also been complaining of productive cough since 2 days
Orthopedics department advised for derotation boot for her right lower limb.
Her diagnosis :
LAD ISCHAEMIA
RIGHT ITC FRACTURE
RIGHT LUNG PNEUMONIA
HYPOALBUMINAEMIA
RENAL FAILURE WITH ANEMIA OF CHRONIC DISEASED
Day 4:
Ward 15
75yr old women
Rt IT fracture
Rt lung pneumonia
CKD with Hydronephrosis
ACD
LAD territory hypokinesia
HTN since 3yrs
Pain at fracture site reduced, feeling better, no fever spikes
I/0 2600/1700
O/E pallor +
PR 96
BP 130/80
Skin traction intact
Cvs:s1 s2+
RS fine crepts +in rt IAA
Abdomen soft non tender
Under C arm: greater trochanteric fracture seen
Plan of ortho people ORIF with PFN or DHS
1unit prbc transfusion was done yesterday. Hemogram sent today report awaited.
Review 2d echo, cardiology fitness and physician fitness to be done.
Patient attendors are explained about the need for 3donors.
75 year old women
Right It fracture
Pod - 1 ORIF with DHS(right)
No fresh complaints, no fever spikes
I/O:1300/900
PR :88/min
BP:100/70
RR:20 cpm
Sp O2 :92%on room air
Cvs:s1 s2+, no murmurs
Rs:BAE+, fine crepts in right IAA.
PA:soft, NT
CNS:No FND
L/E:drain insitu
No soakage
Distal pulses felt
Active ankle and toe movements present
Intraoperatively:
Inj. 0.5% bupivacaine
Inj. fentanyl were given
OT notes:
Pre-operative diagnosis: Right IT fracture
Surgery proposed: ORIF and DHS on the right side
Procedure consent: yes
Blood transfusion consent: yes
Medical or Cardiology clearance: yes
Surgery executed: ORIF and DHS on right side
Implants used: 5 holed DHS, 80 mm Lag screw
Type of procedure: major
Anesthesia: CSE
Time of starting: 12:40 pm
Time of completion: 5:15 pm
Operative procedure: The patient is in combined spinal epidural anesthesia on traction table fracture reduced on traction and internal rotation. A 20 cm incision was given on lateral aspect of right thigh. 100 ml of serous discharge was drained and sent for culture and sensitivity and tissue was sent for biopsy. The fracture site was identified and reduced with the help of bone spikes and there was severe comminution of Greater trochanter and bone loss over the superolateral aspect of the neck of femur. A guide wire was passed into the head of femur in center to center position, triple rearing was done over the guide wire. Then, the 80 mm lag screw was inserted, 140 degrees DHS barrel plate was inserted, reduced to the shaft and fixed with 5 appropriate sized cortical screws. Then, thorough wound wash was given. G bone was inserted into the bone defect and greater trochanter was sutured. The wound was closed in layers over a drain. Sterile dressing was applied and the patient was shifted to post-op in stable condition.
Post op:
NBM till 11:30 pm
IVF NS/RL @80 ml/hr
Inj magnex forte 1.5gm IV BD
Inj metrogyl 100ml IV TID
Inj neomol 100 ml IV TID
Inj Pan 40 mg IV OD
Inj Tramadol 50 mg IV in 100 ml NS SOS for pain
Tab Chymoral forte TID after NBM break
1unit PRBC was transfused intraop.
1unit PRBC was transfused on POD 1.


















Comments
Post a Comment